Pneumothorax In Newborn Survival Rate
Significantly higher mortality rates were found in infants with pneumothorax than in those without pneumothorax. The mortality rates for neonatal pneumothorax are estimated to range from 16% to 65 percent [22, 29–30, and 22–29–31].
Understanding Pneumothorax
Pneumothorax is a medical issue that is characterized by the form of air inside the pleural cavity. This is the lung space as well as the chest wall. This buildup of air can cause the lungs to collapse in part or completely, causing breathing problems and even life-threatening complications. In the article below, we’ll explore the causes of the condition, symptoms, diagnosis, and treatment for pneumothorax.
Causes
Pneumothorax may occur at any time without obvious reason or result from injury or lung conditions. The most frequent cases of spontaneous pneumothorax are in patients with lung disorders like chronic obstructive pulmonary disease (COPD) or cystic fibrosis. It could also be connected with small ruptures of small air sacs, referred to as bullae or blebs. These are more common among smokers.
On the contrary, traumatic pneumothorax is triggered by a physical injury to the chest, like a fractured rib or perforating wound. It can occur in automobile accidents, falls, and gunshot injuries. In addition, medical procedures that require the placement of a catheter or needle in the lungs, for example, lung biopsy or the installation of a central vein catheter, could cause pneumothorax.
Symptoms
The signs and symptoms of pneumothorax differ in proportion to the degree of lung collapse and other elements. The most frequent signs and symptoms include abrupt, painful, or stabbing chest discomfort, which worsens when breathing; shortness of breath; rapid breathing; and an increased heart rate. In some instances, pneumothorax may cause blue skin discoloration, which indicates a deficiency of oxygen in the blood. Patients might be afflicted with anxiety, restlessness, and fatigue.
Diagnosis
To determine if you have a pneumothorax, healthcare specialists typically begin by conducting a thorough physical exam that includes monitoring the lungs for unusual breath sounds. Chest X-rays are often used to verify the diagnosis and determine the extent and position of the pneumothorax.
In some instances, computed tomography (CT) scans or ultrasounds can be conducted to obtain more detailed pictures. If the pneumothorax is believed to be due to an underlying lung disease, further tests for lung function or genetic tests might be carried out.
Treatment
The treatment for pneumothorax is based on the degree of severity of the problem and the reason for it. Minor pneumothoraces that cause significant symptoms can be treated independently without intervention. However, more severe cases usually require medical attention. A common method is to insert a small needle or tube in the chest cavity to take out the excess air and let the lung expand again. This is referred to as chest tube insertion or needle aspiration.
In certain instances, surgery is needed to fix any lung injury and prevent pneumothorax. It can be done with procedures like pleurodesis, where the pleura layers (the membranes surrounding the lung) are joined, or thoracotomy. It involves cutting a bigger cut through the chest to gain access to and repair the lung.
Risk Factors For Newborn Pneumothorax
The condition of newborn pneumothorax is characterized by the form of air within the pleural cavity in the newborn’s chest. It results from an unbalanced buildup of lung air inside the wall, which can impair breathing and cause lung collapse. We will look at the risk factors for newborn pneumothorax. We will also discuss the indications, signs, diagnostics, treatment, and prevention strategies.
Prematurity
Premature infants are more susceptible to developing pneumothorax because their lungs are underdeveloped. The lung tissue is not mature, and insufficient surfactant, a chemical that keeps the lungs open, could make premature babies more prone to lung leaks and air collapse.
Respiratory Distress Syndrome (RDS)
Respiratory stress syndrome (also referred to as hyaline membrane disorder) is a frequent occurrence among premature infants. It is caused by the absence of surfactant in the lungs. This causes difficulty breathing and a higher chance of pneumothorax.
Assisted Ventilation
Newborns who require mechanical ventilation for their newborn, like continuous positive airway pressure (CPAP) and mechanical ventilation via the endotracheal tube, are at greater risk of suffering from pneumothorax. The pressure used during assisted ventilation may result in air leaks, resulting in lung collapse.
Birth Trauma
Birth trauma, particularly during a long or difficult birth, may increase pneumothorax in newborns. Traumas to the chest region, including excessive or prolonged compression, could cause air to enter the pleural cavity and result in the collapse of the lungs.
Infections
Certain diseases, like sepsis or pneumonia, may cause lung tissue to weaken and increase the risk of pneumothorax in infants. Infections can trigger inflammation and injury to the delicate lung structures, which are more vulnerable to air leaks.
Meconium Aspiration Syndrome (MAS)
Meconium aspiration syndrome can occur when a newborn breathes meconium (the baby’s first stool) into the lungs before or after birth. It can lead to airway obstruction, lung inflammation, and an increased chance of having a pneumothorax.
Symptoms And Diagnosis
The signs and symptoms of pneumothorax in newborns vary according to the extent of the problem. Common symptoms include a rapid rate of breathing, grunting sounds when breathing, chest retractions (visible pulling up of the chest wall while breathing), anxiety (bluish skin coloration), and decreased breath sounds on the opposite side of the chest.
To identify newborn pneumothorax, healthcare professionals examine the body and can request diagnostic tests. Chest X-rays are typically utilized to determine whether air is inside the pleural cavity and the extent of lung collapse. Ultrasound imaging is also utilized to detect pneumothorax and help determine the position of a chest tube if one is required.
Treatment
The severity of the problem and the baby’s health will determine the infant pneumothorax treatment strategy. Minor pneumothoraces that are not causing respiratory distress can go away by themselves without intervention. Close monitoring of the baby’s oxygen levels and breathing is vital.
For more severe or symptomatic pneumothoraces, the need for medical intervention is usually the insertion of an insignificant chest tube into the pleural cavity to eliminate the trapped air and permit the lung to expand again. Chest tubes are connected drainage systems that help restore your lung’s normal function. In extreme cases, surgery is needed to fix any lung injury and prevent its occurrence.
Identifying Pneumothorax In Newborns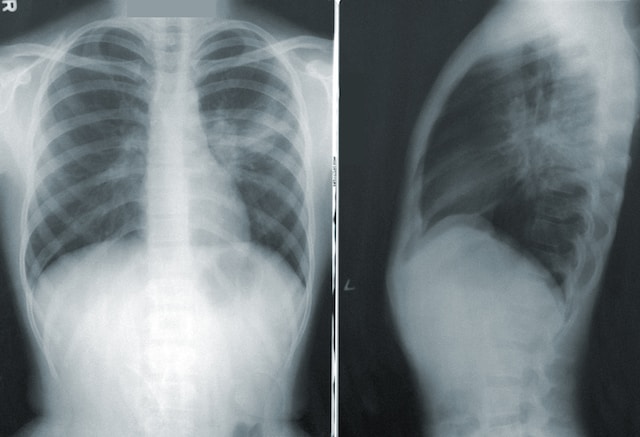
Pneumothorax in infants is a condition that manifests itself as an air pocket within the pleural cavity. This can cause breathing difficulties and lung collapse. It is crucial to recognize the condition early. Essential to ensure prompt treatment and be able to avoid complications. We will examine the different aspects of diagnosing pneumothorax in infants, such as symptoms and diagnosis, treatment, and strategies for prevention.
Treatment Options For Newborn Pneumothorax
The condition of newborn pneumothorax is characterized by the form of air within the pleural cavity. It can lead to respiratory collapse and discomfort. Proper and prompt treatment is crucial to ensuring the health of the infant. We will look at the different treatment options for newborn pneumothorax. These include using a chest tube for conservative treatment, inserting supportive measures, and performing surgical interventions.
Conservative Management
In a few instances, small or asymptomatic pneumothoraces among infants might not require immediate intervention. A conservative approach entails closely monitoring the infant’s health to make sure that the pneumothorax heals on its own without the need for medical assistance. This is usually done when pneumothorax symptoms are small, the baby is healthy, and there are no indications of breathing difficulties. Monitoring is a regular process that includes checking the infant’s vital signs, oxygen saturation levels, and chest X-rays to determine the severity of the airway.
Chest Tube Insertion
For larger or moderately large pneumothoraces, or when breathing difficulties are present and breathing is a problem, insertion into the chest is the main treatment alternative. The procedure involves inserting an insignificant tube inside the pleural cavity to eliminate the accumulation of air and permit the lung to expand again. Chest tubes are attached to a drainage system that takes in air and fluid to facilitate lung expansion. The chest tube insertion procedure is generally performed under local anesthesia, and its efficacy is monitored with regular X-rays and a clinical examination. After the lung has expanded and there’s no sign of air leakage, the chest tube can be safely removed.
Supportive Measures
Alongside chest tube insertion, babies with pneumothorax usually require additional measures to ensure their breathing function and improve their overall health. This may include:
- Oxygen Therapy: Incorporating oxygen into your system can improve oxygen levels and relieve respiratory distress.
- Mechanical Ventilation: In the most severe cases of pneumothorax or if breathing difficulties persist in respiratory distress, mechanical ventilation could be needed. This means using a ventilator to provide breaths to the newborn and help with breathing efforts.
- Continuous Positive Airway Pressure (CPAP): CPAP is a non-invasive method of respiratory support that allows an uninterrupted flow of air pressure to keep the infant’s airways open and enhance the function of the lungs.
- Monitoring: Continuous surveillance of the infant’s vital symptoms, oxygen saturation levels, and the respiratory condition is essential in assessing the effectiveness of treatment and making timely adjustments if required.
Surgical Intervention
Surgery may be required when the chest tube and conservative treatment placement are not effective or if there are other complicating factors. The surgical procedures for infant pneumothorax can include:
Video-Assisted Thoracoscopic Surgery (VATS): VATS is a minimally invasive surgical procedure that allows the surgeon to see the chest cavity with an endoscope-sized camera and specially designed instruments. The surgeon can immediately repair the lung and treat the root causes of the pneumothorax.
Factors Affecting Newborn Survival Rate
The rate at which newborns survive is an important indicator of an entire population’s general health and well-being. Many factors affect the chance of survival for newborns, from maternal health and access to health care to social and environmental conditions. We will look at the various factors that influence the rate of survival for newborns and the importance of addressing these issues to improve the health of infants.
Maternal Health
The mother’s health is essential to the life of the newborn. The maternal factors that influence infant mortality rates are:
- Prenatal Care: A good prenatal routine is vital to detect and treat any risks or issues during pregnancy. Regular check-ups, a healthy diet, and screenings for diseases like gestational diabetes and hypertension can lead to favorable birth outcomes.
- Maternal nutrition: A well-balanced diet and access to adequate nutrition during pregnancy are essential to both fetal and maternal health. A lack of nutrition can cause low birth weight, premature birth, and various other complications that could affect the survival of newborns.
- Maternal age: Moms of adolescents (under 20 years old) and older mothers (over 35 years old) could be at greater risk during pregnancy and birth. These risks can affect the health of the infant and can contribute to increased infant mortality rates.
Access To Healthcare
Access to high-quality healthcare greatly affects the survival rate of newborns. Factors that affect accessibility to healthcare are:
- Highly skilled Birth attendants: the presence of highly skilled health professionals, like midwives or doctors, during the birth process is essential for ensuring that safe births are performed and for immediate treatment for infants in the event of complications.
- Antenatal and postnatal care: Regular and timely appointments with antenatal providers allow early detection and treatment of health problems. Postnatal care visits are essential to the well-being of the newborn and mother in the initial critical days and weeks following the birth.
- Immunizations: Immunizations safeguard newborns from illnesses that are preventable by vaccines and significantly lower the chance of infant death. Immunizations and coverage rates are essential for the health of newborns.
Socioeconomic Conditions
Socioeconomic factors can have a significant influence on the survival of newborns. Important socioeconomic factors include:
- Poverty: Poverty and its problems, like limited access to health care, inadequate nutrition, and poor living conditions, result in higher infant mortality rates. Social support and empowerment programs can address these gaps.
- Education: Mothers’ education plays an important role in infant health outcomes. Educated mothers have a higher likelihood of seeking prenatal treatment, developing healthier habits, and having greater access to the resources needed to improve infant health.
- Infrastructure and Service: Clean water sanitation facilities, transport, electricity, and communications infrastructure are essential in ensuring access to medical and emergency assistance, especially in areas that are rural or not well served.
FAQ’s
Does a baby have an airway?
Air leaks can disappear within a few days with no treatment. Infants with air removed using a catheter or needle usually recover after treatment, provided there aren’t any other lung issues.
What are the long-term effects of pneumothorax on newborns?
What are the long-term consequences? Most of the time, there are no lasting issues once an air leak has been treated. If a trachea tube is required to be employed, a few complications, such as an internal bleed or puncture to the lung, could happen. A few babies with air leaks eventually suffer for a long time from breathing issues.
What Is the Best Way to Manage Pneumothorax in Newborns?
Full-term infants with mild symptoms could be put in a tiny tent inside where oxygen is pumped (an oxygen hood) or given oxygen through two-pronged tubes placed inside the nostrils to breathe in air that has more oxygen than the air in the room.
Can it be treated with pneumothorax without surgery?
Symptoms typically include abrupt chest pain or the feeling of having a short breath. In rare instances, a collapsed lung could be life-threatening. The treatment for a pneumothorax typically involves inserting a needle or an airway between the ribs to eliminate the air. A minor pneumothorax can heal itself.